por
Lauren Dubinsky, Senior Reporter | November 11, 2019
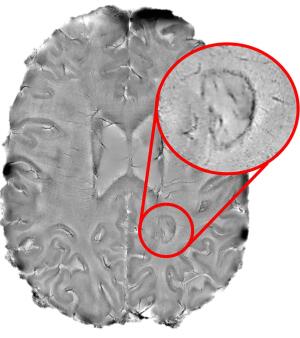
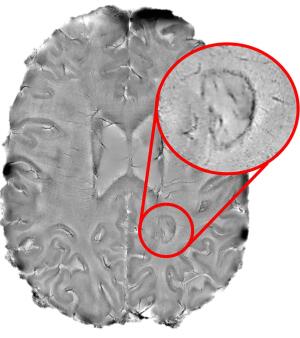
MR images of dark rimmed spots representing ongoing inflammation. Photo courtesy: Reich Lab, NIH NINDS
From the November 2019 issue of HealthCare Business News magazine
MR imaging has a well-established reputation for shedding light on a wide range of medical conditions, but as technology becomes more sophisticated it allows for promising new capabilities. The detection of breast cancer and prostate cancer may drastically improve as more physicians use MR to screen certain patient population and 7T MR is making a big splash in multiple sclerosis (MS) research.
The pros and cons of breast MR
The value of incorporating MR into the breast cancer screening regime has been a subject of debate for years. There isn’t a clear-cut answer, but new research is zeroing in on the patient populations that can benefit the most from this modality.



Ad Statistics
Times Displayed: 123281
Times Visited: 7154 MIT labs, experts in Multi-Vendor component level repair of: MRI Coils, RF amplifiers, Gradient Amplifiers Contrast Media Injectors. System repairs, sub-assembly repairs, component level repairs, refurbish/calibrate. info@mitlabsusa.com/+1 (305) 470-8013
Researchers at the University of Toronto published a study in July that found that annual breast MR screening alone may be more beneficial for women who received thoracic radiation to treat Hodgkin’s lymphoma (HL) as a child. The current guidelines in Ontario call for annual mammograms and MR exams for these women starting at age 30.
Dr. David Hodgson, professor in the department of radiation oncology at the university, explained that there is some evidence that mammography can detect ductal carcinoma in situ (DCIS), which are pre-malignant (and non-fatal) breast lumps often missed by MR.
“Detecting DCIS does not improve survival or reduce breast cancer deaths,” said Hodgson. “Treatment of DCIS does not require chemotherapy whereas invasive breast cancer often does, so it is possible that by detecting DCIS and removing it with surgery, the mammogram may allow a patient to avoid undergoing chemotherapy, but it won’t save her life.”
The study concluded that screening with both mammography and MR starting at age 30 is less effective and more expensive than screening with MR alone. In addition, screening women at age 25 with both modalities instead of mammography alone did not significantly change life expectancy or improve quality of life.
Research like this is important because many female survivors of HL are unaware that they should start breast screening early with MR, and many primary care physicians are also unaware, said Hodgson.
“There are knowledge gaps among stakeholders that likely keep some women from having appropriate screening,” he added.