por
John R. Fischer, Senior Reporter | October 18, 2022
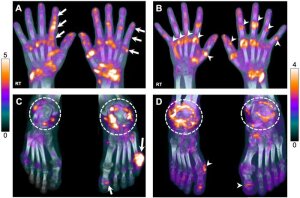
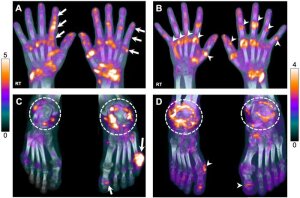
Total-body PET/CT may provide more insights for accurately determining the best course of treatment in people with arthritis. (Photo courtesy of UC Davis)
Total-body PET/CT may offer unknown insights and objective biomarkers for determining appropriate treatments for patients with autoimmune inflammatory arthritides.
Researchers at the University of California-Davis, which helped develop and
install the first U.S.-based total-body PET/CT, saw systemic joint involvement in such patients and found strong correlation between the scanner and joint-by-joint rheumatological evaluations. They also saw moderate to strong correlation with rheumatological outcomes.
Their findings are part of first-in-human research on total-body PET/CT for arthritis, which affects approximately one in four adults (58 million Americans) and is projected to be diagnosed in 78 million by 2040.
“It is unclear which patients should receive which treatments, how exactly these treatments change the inflammatory status of different tissues or outcomes, and the impact the disease and treatments have on other organs of the body,” said Abhijit J. Chaudhari, professor of radiology at UC Davis.
Using an ultralow-dose 18F-FDG total-body PET/CT acquisition protocol, the group scanned 24 patients with AIA and six with osteoarthritis, and also performed joint-by-joint rheumatologic exams. They assessed 1,997 joints in total.
The scan showed 18F-FDG uptake at joints throughout the entire body, including the hands and feet, and did not require custom positioning for patients. Among the AIA group, total-body PET/CT qualitative assessments aligned with the rheumatologic exams for 69.9% of patients.
About 20% had joints that were deemed negative on rheumatological evaluations but positive with the scan. For the remaining 10%, evaluations were positive, while scans were negative.
For the osteoarthritis cohort, results for 91.1% in both exams were in agreement. Joints were negative on rheumatological evaluation but positive on PET/CT for 8.8%. No joints were diagnosed as negative on the scan but positive on the evaluation.
Chaudhari says using total-body PET/CT may improve the ability to assess risk stratification in patients with arthritic disease, as well as select treatments and monitor responses.
“The biomarkers imaged may also have clear potential to accelerate arthritic drug discovery and development. In addition, the inflammatory arthritides assessed in the paper are part of a broad category of autoimmune disorders. This work may contribute to improved understanding of total-body impact on autoimmunity,” he said.
The findings were published
The Journal of Nuclear Medicine.