por
John R. Fischer, Senior Reporter | February 17, 2020
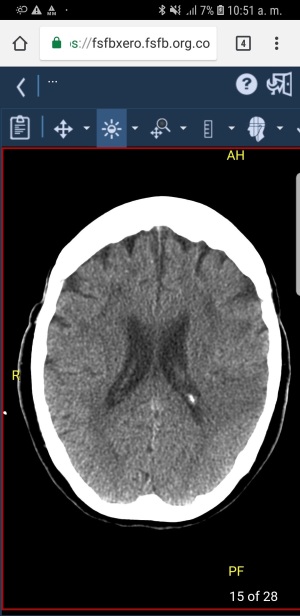
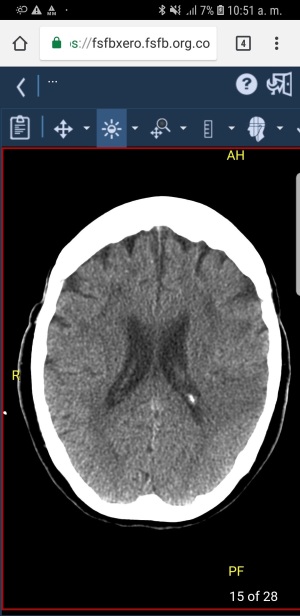
Scans displayed on mobile devices are reliable and accurate for making clinical decisions to assist acute stroke patients, says a new study
Scans displayed on mobile devices are accurate and reliable in clinical settings when having to decide whether or not to administer IV thrombolysis in patients with acute stroke.
That’s what researchers at the University of Los Andes in Bogotá, Columbia found when comparing IV thrombolysis recommendations derived from interpretations of head CT images on smartphone or laptop reading systems, to those made from interpretations of scans within a medical workstation monitor.
“Not only do they improve the availability of images for neuroradiologists, but they also do the same for other medical specialties such as neurologists, emergency physicians and other doctors who have to make decisions in patients with acute stroke (CVA),” Antonio José Salazar, an electrical engineer at the university and an author of the study, told HCB News.



Ad Statistics
Times Displayed: 107305
Times Visited: 6555 MIT labs, experts in Multi-Vendor component level repair of: MRI Coils, RF amplifiers, Gradient Amplifiers Contrast Media Injectors. System repairs, sub-assembly repairs, component level repairs, refurbish/calibrate. info@mitlabsusa.com/+1 (305) 470-8013
To complete their investigation, Salazar and his colleagues developed a web system for mobile decision support devices that implements care and treatment protocols based on recommendations from the American Heart Association and American Stroke Association throughout the patient care and transfer process.
The team used a factorial design of 188 patients, four radiologists, and three reading systems to produce 2,256 interpretations. It then calculated intraobserver and interobserver agreements using the intraclass correlation coefficient (ICC) and five variables for interpretation. These include hemorrhagic lesions; intra-axial neoplasm; stroke dating (acute, subacute, and chronic); hyperdense arteries; and infarct size assessment. Good agreements were observed for all variables, with those necessary to establish contraindications for IV thrombolysis ranked as very good.
Accuracy equivalence tests were also performed for the IV thrombolysis recommendation, taking into account sensitivity, specificity, and the ROC curves. The interobserver agreements for the three reading systems of this evaluation were ranked as very good with an ICC of >0.88. Very good intraobserver agreements were observed for all comparisons at an ICC of >0.84. AUC values (0.83-0.84) and sensitivities (0.94-0.95) for IV thrombolysis recommendation were equivalent among all the reading systems to a 5% equivalent threshold.
Salazar says the findings support the development of mobile-based telestroke services that would increase the availability of neuroradiologists and the possibility of using perfusion therapies in resource-limited countries. This would especially benefit rural facilities that lack specialized doctors to perform CT scans or do not have such personnel 24 hours a day. It would also allow for remote counseling to help in the administration of medicine to break clots — supported by the absence of contraindications in the CT images of the skull — in cases such as hemorrhagic stroke or in the presence of intra-axial neoplasia.
“In our country there are few health institutions that have the possibility of MR or reperfusion CT, and even less with thrombectomy possibilities: of 191 that have intravenous thrombolysis only 14 offer thrombectomy, so intravenous thrombolysis is currently the standard acute treatment in a patient with acute stroke,” said Salazar. “A study could be done evaluating the arteries in angiotac, to identify the site of occlusion, the length of the thrombus and the presence of collaterals to make a thrombectomy decision.”
The findings were published in the
American Journal of Roentgenology (AJR).