por
John R. Fischer, Senior Reporter | August 21, 2018
A new study has found that
discussions between physicians and
patients on lung cancer screenings
are poor in quality
In accordance with national guidelines, physicians are discussing the pros and cons of lung cancer screenings with high-risk patients. They’re just doing it wrong.
That’s the conclusion reached by researchers at the University of North Carolina Lineberger Comprehensive Cancer Center in their new study, which found conversations on lung cancer screening to be "poor" in quality and discussions on the potential harms of screening to be "virtually nonexistent."
"Our payment system rewards procedures and infusions through high levels of reimbursement. Our system does not reimburse well for visits with patients having multiple chronic medical problems in the outpatient setting," senior author Daniel S. Reuland, director of the University of North Carolina Lineberger Comprehensive Cancer Center's Carolina Cancer Screening Initiative and a professor at the UNC School of Medicine, told HCB News. "As a result, visit times are very short, many issues need to be covered quickly, and a culture and practice of moving quickly through visits has developed. This environment is poorly conducive to educating and engaging patients more deeply, and having nuanced, evidence-informed discussions about the trade-offs inherent in many medical decisions."



Ad Statistics
Times Displayed: 75852
Times Visited: 2553 Ampronix, a Top Master Distributor for Sony Medical, provides Sales, Service & Exchanges for Sony Surgical Displays, Printers, & More. Rely on Us for Expert Support Tailored to Your Needs. Email info@ampronix.com or Call 949-273-8000 for Premier Pricing.
More than 234,000 people are diagnosed annually with lung cancer, which takes the lives of more than 154,000 individuals each year, making it the leading cause of death throughout the U.S., according to the American Cancer Society.
Discussions on screenings are recommended to help prevent deaths from occurring, and are even required in some cases by national guidelines. In addition, organizations like the U.S. Centers for Medicare and Medicaid require these conversations to take place before funding such procedures, and to include in them the pros and cons of screening, as well as issues of overdiagnosis and false positives and the risk of total radiation exposure.
Researchers analyzed 14 transcripts of audio-recorded office visit discussions between age-eligible patients and their doctors, finding them to be brief and one-sided, with each physician failing to mention any word on the potential harms involved in screening, the chance for false positives, or the need for additional imaging or invasive diagnostic procedures. Complete conversations for screenings, on average, were found to last one minute.
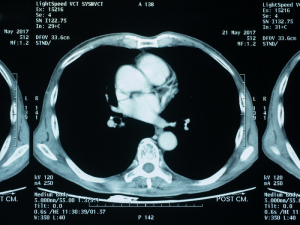
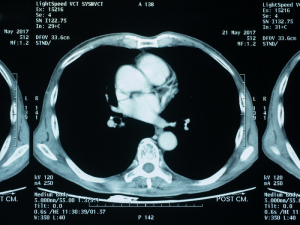
Detection of lung cancer in its earliest stage reduces the risk of death by the disease, according to the National Lung Screening Trial (NLST), which
found that low-dose spiral CT scan screenings resulted in 20 percent fewer lung cancer deaths among those with very high risks than patients who underwent chest X-rays.