Exclusive: Interview with ASTRO Chair Dr. Anthony Zietman
October 03, 2011
This report originally appeared in the October 2011 issue of DOTmed Business News
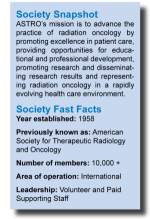
Current chair and immediate past president of the American Society for Radiation Oncology, Anthony Zietman, M.D., recently spoke with DOTmed News about the society’s goals and accomplishments, challenges oncology faces and the differences between U.S. and British health care policies.
DMBN: Dr. Zietman, what attracted you to a career in medicine?
Zietman: If I’m being honest, I believe we’re just leaves in the wind. In Britain where I trained, you go to medical school at 18. Here, you go as an adult and it’s an informed position. You’re good in science and you’re good in math . . . why not go into medicine? I was interested in medicine, but also in politics. I had a notion in my head that I was going to be Prime Minister – 250 people in my class also had that thought – one actually did.
So, I altered my course. That’s another difference – we qualify as doctors at 22 or 23, so we do a lot of residency. So I had five years in medical and radiation oncology. When I came to the U.S. in 1986, primarily to do research, I had to choose and I chose radiation oncology because I thought I could cure more people.
DMBN: Having the background in Britain and years practicing in the U.S., can you explain some of the differences in the health care systems?
Zietman: The National Health Services in Britain were set up in 1947 by a government that did not want to return to how things were before the war. There was a feeling; you had to do right by these people. The Labor government established a national health service over the protests of the doctors. Now, it has become a point of pride in England that everyone is covered. There are no cashiers in hospitals – money isn’t even discussed. The waiting list could be substantial, but it was fair. Today, no British government would dismantle it — it would be political suicide.
Equally when I came to the states, I enjoyed the lavish facilities. I enjoyed not having waiting lists. The system could soak up whatever came its way. If it was more demand than could be met, they hired more doctors or established more hospitals. It could react rapidly to demand and bring in high-tech technology quickly. There was also of course, enormous innovation.
It’s now returning to bite us – so many technologies to choose from – but they’re so expensive with only a marginal benefit to the patient, whereas the British system is doing well, because it hasn’t brought in the radiology technology without first giving it significant scrutiny.
So the main differences are the pride in the National Health Service and evidence-based spending. But Britain is slow to introduce new technology and there is the waiting list.
DMBN: What has been your proudest moment?
Zietman: Prostate cancer specialists have a belief that PSA screening would eradicate the disease. A small group of us have been arguing that overtreatment is a huge problem. Finally, that viewpoint has not only been heard, it’s becoming mainstream. Now, it is not what treatment should I give them, but do they need treatment at all? It is a difficult position to move forward. We have a health care system that rewards for doing things – I earn far more for treating than not treating.
As president of ASTRO,I had the bully pulpit. In 2010 (my year) I had the chance to speak in San Diego to the full group and discuss this. As a free-spending specialty, we need to step back and ask, are we treating the right patients? Do they need to be treated at all? Is the technology REALLY benefitting the patients, or is it just a sexy marketing tool?
There’s a lively debate about what we’re really achieving – about what we can get from the technology and benefitting the patients.
DMBN: Can you share some of the goals you have as chair of ASTRO or accomplished as president?
Zietman: My goal is to make the specialty realize the party is over. We have to regulate ourselves using our consciences, otherwise others will do the job for us. Another goal was to introduce a huge safety campaign: Target Safely. We’ve changed the culture so it really resembles the airlines. There are checklists, anyone from the staff is allowed to speak up, etc. 98.8 percent of oncology is safe. But if 98.8 percent of aircrafts took off and landed safely, that would be unacceptable.
DMBN: What future role do you intend to play in the society?
Zietman: I will be continuing the work on those goals, and be engaged in all those projects. Also, in October, I will be the editor-in-chief of the International Journal of Radiation Oncology.
DMBN: What advice would you offer for individuals looking to pursue a leadership role for ASTRO?
Zietman: Start early. We’re actually encouraging residents to get engaged. Working for your specialty really adds enough dimension to a medical career. You’ll never be bored if you diversify.
DMBN: What do you believe to be the biggest challenges oncology will face in the future?
Zietman: Cost. We have proton beam facilities costing $200 million. New drugs that may be $100,000 for one-year supply that only adds a few months to life. We need a new code of ethics and value that help us prioritize. We have to and are establishing a code of best practices — one toward cost and the other toward evidence. It’s not always easy to find evidence-based [practices] around rarer diseases. It’s going to involve some loss of income. At some subconscious level, having a quarter million dollars in loans leads to a loss of conscience-based medicine.
DMBN: Do you anticipate any major developments in the sector in the near future?
Zietman: If we start practicing according to the evidence, it will be an earthquake. Emphasis on safety, patient outcome, evidence-based outcome and doing the right thing – conscience based medicine. What we don’t want to do is restrain the system so far that we stifle innovation.
Current chair and immediate past president of the American Society for Radiation Oncology, Anthony Zietman, M.D., recently spoke with DOTmed News about the society’s goals and accomplishments, challenges oncology faces and the differences between U.S. and British health care policies.
DMBN: Dr. Zietman, what attracted you to a career in medicine?
Zietman: If I’m being honest, I believe we’re just leaves in the wind. In Britain where I trained, you go to medical school at 18. Here, you go as an adult and it’s an informed position. You’re good in science and you’re good in math . . . why not go into medicine? I was interested in medicine, but also in politics. I had a notion in my head that I was going to be Prime Minister – 250 people in my class also had that thought – one actually did.
So, I altered my course. That’s another difference – we qualify as doctors at 22 or 23, so we do a lot of residency. So I had five years in medical and radiation oncology. When I came to the U.S. in 1986, primarily to do research, I had to choose and I chose radiation oncology because I thought I could cure more people.
DMBN: Having the background in Britain and years practicing in the U.S., can you explain some of the differences in the health care systems?
Zietman: The National Health Services in Britain were set up in 1947 by a government that did not want to return to how things were before the war. There was a feeling; you had to do right by these people. The Labor government established a national health service over the protests of the doctors. Now, it has become a point of pride in England that everyone is covered. There are no cashiers in hospitals – money isn’t even discussed. The waiting list could be substantial, but it was fair. Today, no British government would dismantle it — it would be political suicide.
Equally when I came to the states, I enjoyed the lavish facilities. I enjoyed not having waiting lists. The system could soak up whatever came its way. If it was more demand than could be met, they hired more doctors or established more hospitals. It could react rapidly to demand and bring in high-tech technology quickly. There was also of course, enormous innovation.
It’s now returning to bite us – so many technologies to choose from – but they’re so expensive with only a marginal benefit to the patient, whereas the British system is doing well, because it hasn’t brought in the radiology technology without first giving it significant scrutiny.
So the main differences are the pride in the National Health Service and evidence-based spending. But Britain is slow to introduce new technology and there is the waiting list.
DMBN: What has been your proudest moment?
Zietman: Prostate cancer specialists have a belief that PSA screening would eradicate the disease. A small group of us have been arguing that overtreatment is a huge problem. Finally, that viewpoint has not only been heard, it’s becoming mainstream. Now, it is not what treatment should I give them, but do they need treatment at all? It is a difficult position to move forward. We have a health care system that rewards for doing things – I earn far more for treating than not treating.
As president of ASTRO,I had the bully pulpit. In 2010 (my year) I had the chance to speak in San Diego to the full group and discuss this. As a free-spending specialty, we need to step back and ask, are we treating the right patients? Do they need to be treated at all? Is the technology REALLY benefitting the patients, or is it just a sexy marketing tool?
There’s a lively debate about what we’re really achieving – about what we can get from the technology and benefitting the patients.
DMBN: Can you share some of the goals you have as chair of ASTRO or accomplished as president?
Zietman: My goal is to make the specialty realize the party is over. We have to regulate ourselves using our consciences, otherwise others will do the job for us. Another goal was to introduce a huge safety campaign: Target Safely. We’ve changed the culture so it really resembles the airlines. There are checklists, anyone from the staff is allowed to speak up, etc. 98.8 percent of oncology is safe. But if 98.8 percent of aircrafts took off and landed safely, that would be unacceptable.
DMBN: What future role do you intend to play in the society?
Zietman: I will be continuing the work on those goals, and be engaged in all those projects. Also, in October, I will be the editor-in-chief of the International Journal of Radiation Oncology.
DMBN: What advice would you offer for individuals looking to pursue a leadership role for ASTRO?
Zietman: Start early. We’re actually encouraging residents to get engaged. Working for your specialty really adds enough dimension to a medical career. You’ll never be bored if you diversify.
DMBN: What do you believe to be the biggest challenges oncology will face in the future?
Zietman: Cost. We have proton beam facilities costing $200 million. New drugs that may be $100,000 for one-year supply that only adds a few months to life. We need a new code of ethics and value that help us prioritize. We have to and are establishing a code of best practices — one toward cost and the other toward evidence. It’s not always easy to find evidence-based [practices] around rarer diseases. It’s going to involve some loss of income. At some subconscious level, having a quarter million dollars in loans leads to a loss of conscience-based medicine.
DMBN: Do you anticipate any major developments in the sector in the near future?
Zietman: If we start practicing according to the evidence, it will be an earthquake. Emphasis on safety, patient outcome, evidence-based outcome and doing the right thing – conscience based medicine. What we don’t want to do is restrain the system so far that we stifle innovation.